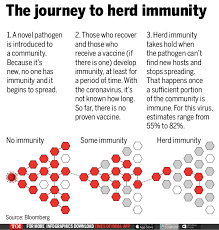
Covid-19 Herd Immunity. Three months later, the British experience demonstrates that herd immunity is difficult in the face of the highly transmissible Delta form of the coronavirus. Covid-19 instances and fatalities have increased in recent weeks as winter approaches. The main line is that relying on immunity, which is flawed to begin with and deteriorates with time, does not ensure a speedy triumph against Delta.
The limitations were lifted “in the expectation that vaccines and natural immunity would prevail quite swiftly,” according to Tim Spector, professor of genetic epidemiology at King’s College London. “What has been demonstrated is that this alone does not work.”
On Wednesday, the government reaffirmed its policy of using vaccinations as its primary defence, saying it did not see the need to implement other measures such as face-mask regulations and proof-of-vaccination documentation, which some physicians and scientists believe are required.
When the government of England discontinued mandatory mask wearing and social separation on July 19, an early vaccine rollout combined with high infection rates earlier in the epidemic meant that Britain seemed to have a high degree of protection. In much of the United Kingdom, a survey at the time suggested that about 90% of people aged 16 and up had antibodies against the virus, either via vaccination or prior infection.
They’re getting closer to 50,000 now. According to Oxford University’s Our World in Data, the daily average has reached about 667 per million. This contrasts to 80 million in France and 147 million in Germany, both of which use vaccination certificates and other procedures. Last month, Britain began giving immunity supplements to those aged 50 and above, as well as those with specific health problems, in an effort to improve immunity.
Over the last week, hospitalizations have increased by 10%. The use of vaccines has greatly decreased the chance of mortality. According to Our World in Data, daily Covid-19 fatalities are about two per million on average, much lower than the eight per million when infection levels were around the same level in early January. Nonetheless, the mortality toll in the United Kingdom is about four times that of France, where fatalities average 0.47 per million, and more than double that of Germany, where deaths average 0.82 per million.
Few limitations, diminishing protection from vaccination, a slowing vaccine campaign, a large number of unvaccinated children, and increased indoor mixing are all probable contributory factors to the persistently high and growing illness rates in the United Kingdom, according to epidemiologists.
Despite a promising start, the United Kingdom’s vaccine rollout has lagged behind that of its European counterparts, owing to weaker demand from younger individuals. While more over 90% of individuals aged 60 and up have been immunised, the rate declines to less than 70% among those aged 35 and younger. Younger individuals are also more prone to visit crowded locations, which means that the least vaccinated persons are likely to contribute disproportionately to the spread of the virus, according to Bill Hanage, an associate professor of epidemiology at Harvard University.